Anti-Tubercolusis drugs, Pharmacology III, Unit 3 Download Notes PDF BPharmacy 6th Semester 2022
📑 BP602T Pharmacology III
| Title: |
Anti-Tubercolusis drugs, Pharmacology III, Unit 3 |
| Course: | BPharmacy |
| Semester/Year: | 6th Semester |
| Subject: | BP602T Pharmacology III |
| Session: | 2022 |
| Category: | Notes |
| Pharmacology BPharmacy BPharm 6th Semester Important Exam Notes | |
You can download BPharmacy Notes & Previous Year's Question Paper from here. All semester-wise Notes & Previous Year Question Papers are available on HK Technical. You can download all question papers & notes for BPharmacy all semester/years for free.You can view All Question Papers From Here.
👉 Download All Question Papers for BPharmacy
👉 Premium Question Paper/Notes Library
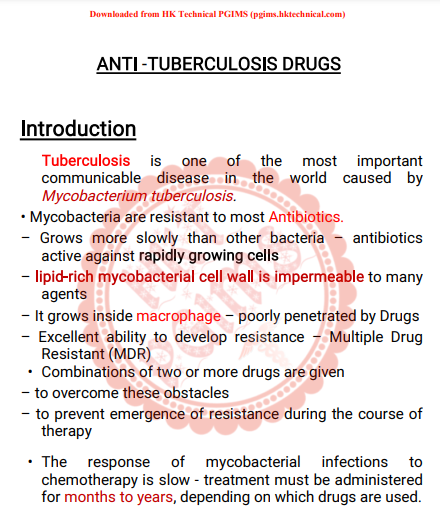
ANTI -TUBERCULOSISDRUGS
Introduction
Tuberculosis is one of the most importantcommunicable disease in the worldcausedbyMycobacterium tuberculosis. • Mycobacteria are resistant to most Antibiotics. – Grows more slowly than other bacteria–antibioticsactive against rapidly growing cells – lipid-rich mycobacterial cell wall is impermeabletomanyagents – It grows inside macrophage – poorly penetratedbyDrugs– Excellent ability to develop resistance–MultipleDrugResistant (MDR)
• Combinations of two or more drugs aregiven– to overcome these obstacles – to prevent emergence of resistance duringthecourseoftherapy
• The response of mycobacterial infectionstochemotherapy is slow - treatment must beadministeredfor months to years, depending on whichdrugsareused.Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
Symptoms of an active TB infection include: • Cough that lasts for three weeks or more• Coughing up blood
• Chest pain
• Fever
• Fatigue
• Night sweats
• Unexplained weight loss
• TB is a highly infectious disease whichgenerallyspreadsby coughing as it releases the virus inair dropletsorwhen a healthy person comes in contact withapatient.TB types: • Pulmonary Tuberculosis (Mainly effect lungs)
• Extra-pulmonary Tuberculosis (effect bones, peritoneum,brain)
Tuberculosis can be detected by: • Sputum test • X-ray
Classification of TB drugs:
According to clinical utility the anti TBdrugscanbeDownloaded from HK Technical PGIMS (pgims.hktechnical.com)
divided into 2 groups – First Line : high anti-tubercular efficacy aswell aslow toxicity: routine drugs. Isoniazid (H)
Rifampin (R)
Pyrazinamide (Z)
Ethambutol (E)
Streptomycin (S) (HRZES)
Second Line : low anti-tubercular efficacy or highertoxicity-reserve drugs
• Ethionamide (Eto)
• Prothionamide (Pto)
• Cycloserine (Cs)
• Para-aminosalicylic acid (PAS)
• Rifabutin
• Thiacetazone (Thz)
Fluoroquinolones: • Ofloxacin (Ofx), Levofloxacin (Lvx/Lfx), Moxifloxacin(Mfx), Ciprofloxacin (Cfx)
Injectable drugs
• Kanamycin (Km), Amikacin (Am), Capreomycin(Cm)Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
• TB medications are supplied by DOTScentreinthedesignated hospitals and community centreinIndia.Isoniazid (H)
• Named as Isonicotinic acid hydrazide
• Most active drug for the treatment of tuberculosis• freely soluble in water
• tuberculocidal for actively growing tuberclebacilli • penetrates into macrophages and is activeagainstbothextracellular and intracellular TB organisms. Mechanism of Action & Basis of Resistance: • inhibits synthesis of mycolic acids –whichareuniquefatty acid components of mycobacterial cell walls.• Highly selective for mycobacterium• Resistance – Always given in combination, if given aloneonlythebacillihave chances to develop resistance. Pharmacokinetics
• readily absorbed orally and diffuses intoall bodytissues.• metabolised in liver: acetylation by N–acetyltransferase.• Half-lives : 1 hour(fast acetylators)
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
3 hours (slow acetylators)
• Excreted mainly in the urine. • Contraindicated - severe preexisting hepaticinsufficiencyDosage: • Typical dosage of isoniazid is 5 mg/kg/d–10mg/kg/d(sever infection) or 15 mg/kg dose –twiceweekly• Adult dose : 300 mg oral dose O.D. • Pyridoxine (Vit-B6) given prophylactically(10mg/day)prevents the neurotoxicity even with higher doses.Peripheral neuritis and a variety of neurologicalmanifestations (numbness, mental disturbances, rarelyconvulsions), hepatitis (in adult) are themost importantdose-dependent toxic effects. Rifampin (Rifampicin, R)• Semi-synthetic derivative of rifamycinBproducedbyStreptomyces mediterranei. • Rifampin is bactericidal to M. tuberculosisandmanyother gram-positive and gram-negativebacterialikeStaph. aureus, N. meningitidis, H. influenzae. • Effectiveness against TB is same as isoniazid.
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
• Both extra- and intracellular organismsareaffected.Ithas good sterilizing and resistance preventingactions.Mechanism of Action & Resistance: • Binds to the bacterial DNA-dependent RNApolymerase-inhibits RNA synthesis, thus polymerizingfunctionisblocked. • Resistance: mutations of gene result inreducedbindingof rifampin to RNA polymerase, thus produceresistance.Pharmacokinetics: • It is well absorbed orally, but food decreasesabsorption;so rifampin is to be taken in empty stomach. • Metabolised in liver and excreted mainly throughbileandurine. • The t½ of rifampin is variable (2–5 hours). Dosage: • 10 mg/kg/d O.D. for 6 months incombinationwithisoniazid or other antitubercular drugstopatient.• Some atypical mycobacterial infectionsandinleprosyDownloaded from HK Technical PGIMS (pgims.hktechnical.com)
• 600 mg twice daily for 2 dayscaneliminatemeningococcal carriage
• 20 mg/kg/d for 4 days - prophylaxisincontactsofchildren with Haemophilus influenzae. Adverse reactions: • Urine and secretions may become orange-red—butthisis harmless. • Hepatitis (occurs in pre-existing liver diseaseandisdose-related)
• Jaundice
• Occasional adverse effects include: rashes, flu-likesyndrome characterized by fever, chills, myalgia, nausea,vomiting. Ethambutol (E)
Synthetic, water-soluble, heat-stable compound- dispensedas the dihydrochloride salt. • Tuberculostatic in nature. • Given in combination with RHZ, it hasbeenfoundtohasten the rate of sputumconversionandtopreventdevelopment of resistance. Mechanism of action:
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
• Inhibits mycobacterial arabinosyl transferases-anessential component of mycolic acidinmycobacterialcell wall synthesis. • Resistance – due to alteration in target gene• No cross resistance with other anti-tubercular drug.Pharmacokinetics
• About 3/4 of an oral dose of E is absorbed. • Temporarily stored in RBC
• It is excreted in urine by glomerular filtrationandtubularsecretion; plasma t½ is ~4 hrs. • Caution taken for renal failure patient
Dosage: Ethambutol hydrochloride - 15–20mg/kg/O.DAdverse Reactions
• Loss of visual acuity/colour vision, fielddefects(lossofpart of the usual field of vision) due toopticneuritisisthe most important toxic effect. Patientsareadvisedtostop the medication, once they report suchproblems.• Permitted in children but with precautions. • It produces few other symptoms: nausea, rashes, fever,rarely peripheral neuritis (damage innervesignalfrombrain), hyperuricemia.
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
Pyrazinamide(Z)
• It is chemically similar to isoniazid, andwasdevelopedin 1952. • It is weakly tuberculocidal and moreactiveinacidicmedium. • It is more lethal to intracellularly locatedbacilli. • Highly effective during the first 2 monthoftherapy.Reduce the treatment duration and chanceof relapse.Mechanism of Action
• Pyrazinamide is converted to pyrazinoicacid(activeform) - by enzyme pyrazinamidase. • Disrupts mycobacterial cell membranemetabolismbyinhibiting mycolic acid synthesis. • Resistance develops if: –pyrazinamide is taken alone. – mutations of the enzyme causingconversionofpyrazinamide to its active form. Pharmacokinetics
• Pyrazinamide is absorbed orally andwidelydistributed,has good penetration in CSF, becauseof whichitishighly useful in meningeal TB (brain TB).
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
• extensively metabolized in liver andexcretedinurine;plasma t½ is 6–10 hours. • Dosage: 20–30 mg/kg OD or 30-40 mg/kg; 3timesperweek dose. Adverse effect:
Hepatotoxicity (in 1–5% of patients) –lesscommoninIndian population. • Abdominal distress, arthralgia (joint pain), flushing,rashes, fever and loss of diabetescontrolandhyperuricemia are other adverse effects. • Contraindicated in liver disease patient. Streptomycin• Class of aminoglycoside antibiotic. • First clinically useful anti-tubercular drug. • It is tuberculocidal, but less effectivethanINHorrifampin. • Acts only on extracellular bacilli –poor penetrationintocells
• Doesn’t cross the BBB, but penetrates tubercularcavities.Mechanism of action: • Irreversible inhibitors of protein synthesis,
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
• Bactericidal • Inside the cell, aminoglycosides bindtospecific30S-subunit ribosomal proteins andinhibitsproteinsynthesis. • Dosage: Adults: 20–40 mg/kg/daily for 2months.• Adverse Reactions
Ototoxic, nephrotoxic, vertigoandhearinglossare the common adverse effectsandmaybepermanent. SecondLineDrugsThese drugs are considered only when – resistance to one or more 1st line drugs. – Serious treatment-limiting adverse drugreactions• Expert guidance to deal with the toxic effectsisrequiredEg: Paraminosalicylic Acid, Cycloserine, Kanamycin,Amikacin, Ciprofloxacin, Olfloxacin, Clarithromycin,Azithromycin
Para-aminosalicyclicAcid(PAS)• Introduced in 1946, PAS is related tosulfonamidesandacts probably by the same mechanism, i.e. inhibitionofDownloaded from HK Technical PGIMS (pgims.hktechnical.com)
folate synthase. • highly specific for M. tuberculosis. • PAS is tuberculostatic and one of the least activedrugs.• limited to the treatment of MDR tuberculosis. • Adverse effects:anorexia, nausea, epigastricpain,rashes, fever, malaise, hypokalaemia, goiter, liverdysfunction etc. • Dose: 10–12 g (200 mg/kg) per day individeddoses;Ethionamide(Eto)
• It is a moderate efficacy anti -Tb drug, actsonbothextra-and intracellular bacilli. • Chemically related to isoniazid, worksbyblockingthesynthesis of mycolic acids. • Dosage of 15 mg/kg/d - initial dose of 250mgoncedaily.• AE: Anorexia, salivation, metallic taste, epigastricdiscomfort, sulfurous belching (burpsthat smelllikerotten eggs) and hepatitis. It also causesachesandpains,peripheral neuritis, behavioural changes, rashes,impotence, menstrual disturbances andgoiteronprolonged use.
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
Capreomycin(cm)
• it is a peptide protein synthesis inhibitor antibioticobtained from Streptomyces capreolus. • Dose: 0.75–1.0 g/day i.m. • treatment of drug-resistant tuberculosis. • Strains of M tuberculosis that areresistanttostreptomycin or amikacin are susceptibletocapreomycin. • Nephrotoxic and ototoxic, eosinophilia(highereosinophils), rashes, fever and injectionsitepainoccurs.Kanamycin (Km), Amikacin(Am)• These are tuberculocidal aminoglycosideantibiotics.• Treatment of tuberculosis suspectedor knowntobecaused by streptomycin-resistant or multi-drugresistantstrains
• Kanamycin is more toxic comparatively toamikacin,butin RNTCP Km is preferred because it is cheap. • Both Km and Am produce less vestibular toxicitythanhearing loss, but are equally nephrotoxic. • Dose: 0.75–1.0 g/day (10–15 mg/kg/day) i.m.
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
Fluoroquinolones(FQs)• In addition to their activity against manygram-positiveand gram-negative bacteria, FQs inhibit strainsofM.tuberculosis
• FQs are a key component of all regimensforMDR-TB,except
when bacilli are found to be resistancetothem. • Standard dosage – Ciprofloxacin: 750 mg orally twice a day – Levofloxacin: 750 mg once a day – Moxifloxacin: 400 mg once a day
SHORT COURSE CHEMOTHERAPY• After several years of trial, the WHOintroduced6–8month multidrug ‘short course’ regimensin1995underthe DOTS programme. • Cases are divided into 4 categories: • Category I: New case of sputumsmear +veorseverepulmonary TB, or severe forms of extrapulmonaryTB(meningitis, etc.). • Category II: Defaulted, irregularly treatedandrelapseDownloaded from HK Technical PGIMS (pgims.hktechnical.com)
cases. • Category III: New sputumsmear –ve pulmonaryTBandless severe forms of extrapulmonary TB(glandular/skinTB, etc.). • Category IV: Chronic cases who remainedoragainbecame sputum smear +ve after receivingfullysupervised category II treatment. Multidrug-resistant TB(MDRTB)• Drug resistance emerges when anti-TBmedicinesareused inappropriately, through incorrect prescriptionbyhealth care providers, poor quality drugs, andpatientsstopping treatment prematurely. • Multidrug-resistant tuberculosis (MDR-TB) isaformofTBcaused by bacteria that do not respondtoisoniazidandrifampicin, the 2 most effective first-lineanti-TBdrugs.MDR-TB is treatable and curable by usingsecond-linedrugs.
Downloaded from HK Technical PGIMS (pgims.hktechnical.com)
📝 BP602T Pharmacology III
📝 BPharmacy 6th Semester Notes
📝 Download Previous Year's Question Papers
📝 Download Notes PDF
📝 Download Handwritten Notes
📝 Download BPharmacy Question Papers
📝 Download B.Sc. Nursing Question Papers
📝 Download Last Year's Question Papers
📝 BPharmacy All Semester PDF Download
📝 Download PDF Notes as per Latest PCI Syllabus Pattern
📝 Download B.Sc. Nursing Notes as per latest syllabus pattern
📝 Download All Previous Years Question Papers
📝 PGIMS Rohtak Question Papers
📝 AIIMS Question Papers
📝 B.Sc. Nursing Question Papers
📝 B.Tech Question Papers
📝 Download Free PDF Notes



Post a Comment
0 Comments